This article will explain about Lung Transplant for Mesothelioma. Lung transplants become a necessary survival option for mesothelioma patients when a person’s respiratory system has been damaged to a level where he/she will not be able to live without a replacement lung.
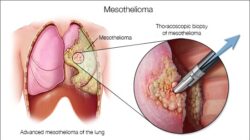
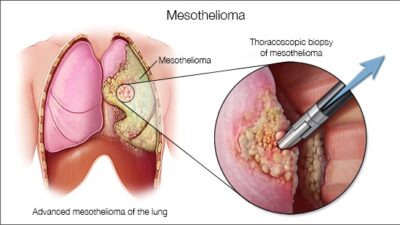
For instance in a disease known as pulmonary fibrosis, the lungs become so scarred such that their air sacs are replaced with fibrotic tissues.
These tissues accumulate in masses and lose the lung’s ability to transfer oxygen into the bloodstream. It is of utmost important that the lungs be able to transfer oxygen to the rest of the body via the bloodstream and when this is interrupted, the patient’s life is threatened.
Once the lungs become extremely scarred, there is no reversal, meaning they cannot heal themselves; thus a lung transplant will be necessary. A lung transplant surgery is a complicated task and can only occur when the right donor is available.
The donor’s lungs are carefully removed and immediately transported to the hospital where the receiving patient is being cared for.
Since lungs can only be preserved for 5-6 hours, it is important that once they are extracted from the donor’s body, they be immediately delivered to the receiving patient.
How Is a Lung Transplant Performed?
A lung transplant surgery is performed under general anesthesia where the patient is lifeless and cannot feel any pain.
The recipient’s heart is stopped and an artificial breathing machine is used to maintain the body’s stasis. An incision is made through the breast bone and a heart-lung bypass machine controls the blood circulation and provides oxygen levels to the body.
Once the patient’s heart and lungs are removed, the donor’s heart and lungs are stitched into place. After this, the heart-lung bypass machine is disconnected and blood flows through the donor’s heart and air flows in to the donor’s lungs.
The patient will have to stay under intensive care unit for several days as any heart failure risk is fatal. The image above shows vascular attachments where new transplanted lungs & heart are stitched into the receiving patient’s body.
A lung transplant surgery is recommended for patients with severely diseased lungs or severely damaged heart or both. It is not recommended for patients with poor kidney or liver functions.
The risks for taking the general anesthesia include breathing problems & reactions to medications. Risks for the surgery itself include infection & excessive bleeding.
More risks for the lung transplant surgery are:
– Failure of the donor’s lungs & heart
– Rejection of any transplanted organs
– Infection caused by taking anti-rejection (immunosuppression) medicine
– Stroke
– Blood clots
Are You Eligible for Lung Transplant Surgery?
Your eligibility for lung transplant surgery will be assessed and examined by a few parties including:
– A pulmonologist (lung specialist)
– Your surgeon
– Your family doctor
– Lung Transplant coordinator
If you are approved for a lung transplant surgery, you will have to go on a waiting list for several months to 1-2 years. Furthermore, it is also important to know that you will have to take medications for the rest of your life to keep your body from rejecting the new transplated lungs.
An example of such drugs include cyclosporine and corticosteroids.
Here are the list of symptoms that might cause you discomfort a few weeks after the lung transplant surgery is complete:
– Rapid weight loss
– Chest discomfort
– Chronic dry cough
– Weakness or feeling of fatigue
– Shortness of breath
Prognosis
A heart transplant surgery is only conducted if the chances of success are really high. It is estimated 40% – 50% of patients can live for another 4-5 years.
Some of the setbacks for success of a heart transplant surgery include finding the right donor, the chance for the body to reject the new transplanted lungs/heart, and the cost of surgery & medications.
Recovery period after surgery is normally 6 months and the patient will have to undergo many x-rays during this time.
dr. Bulawan